With so many unfamiliar words and phrases associated with progressive keratoconus, it might be difficult to keep them all straight! You may be curious what keratoconus is, what the different types of lenses and treatment options are, what the tests you may be receiving are, or who the different physicians are that you’re referred to. We know keeping track of everything you learn when it comes to your keratoconus journey can be a challenge, so we want to help!
We’re defining some of the key terms that someone who is newly diagnosed with the progressive disease should be aware of. Some of them you may already know, but there’s probably others that you’re not familiar with at all.
Keratoconus
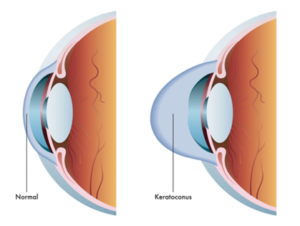
Keratoconus (often referred to as ‘KC’ or ‘KCN’) is a sight-threatening eye disease in which the cornea weakens and thins over time, causing the development of a cone-like bulge and optical irregularity of the cornea. Keratoconus can result in significant visual loss and may lead to corneal transplant in severe cases.

Corneal Cross-Linking
Corneal Cross-Linking: Corneal collagen cross-linking is a minimally invasive outpatient procedure to slow or halt the progression of keratoconus.
Epi-Off Cross-Linking: Epi-off cross-linking requires the removal of the epithelium, the outermost layer of the cornea, to assure deep penetration of the riboflavin eye drops. iLink® epi-off cross-linking performed with Photrexa® Viscous (riboflavin 5’-phosphate in 20% dextran ophthalmic solution), Photrexa® (riboflavin 5’-phosphate ophthalmic solution), and the KXL® system has been rigorously tested and is the ONLY cross-linking procedure approved by the US Food and Drug Administration (FDA). iLink is also the only cross-linking procedure that is eligible for insurance coverage.
Epi-On Cross-Linking & Holcomb C3R: Epi-on cross-linking is an investigational procedure where the epithelium is left intact. There are currently no FDA-approved epi-on cross-linking procedures in the U.S. Holcomb C3R is a marketing trademark for an epi-on cross-linking procedure. Neither the drug nor device used in the Holcomb C3R procedure is FDA-approved for use in corneal cross-linking and are not covered by insurance.
Additional Treatment Options
The following treatments do not slow or halt keratoconus progression and are intended to address the vision needs of keratoconus.
Eyeglasses or Soft Contact Lenses: Mild and early cases of keratoconus can be managed with glasses or traditional non-specialty soft contact lenses if the degree of corneal distortion is not too severe. Typically, in these cases, soft astigmatism-correcting contact lenses are required. More advanced cases can be treated with specialty soft lenses, designed specifically for keratoconus. These lenses typically have a thick central optic zone to mask the corneal irregularity and a thin periphery for comfort. Cases of moderate and somewhat severe keratoconus may be treated with these specialty lenses. These lenses are limited in terms of whether they can provide adequate vision correction for the individual, especially as the condition progresses.
Rigid Gas Permeable (RGP) Contact Lenses: RGP lenses are rigid lenses made of durable plastic that can transmit oxygen. RGP lenses can be custom designed for the shape of a person’s cornea and are easy to apply, remove, and care for.

Scleral Contact Lenses: Scleral lenses are a type of RGP contact lens that people with keratoconus often wear. These lenses, which are made of durable plastic that can transmit oxygen, are larger in diameter than other RGPs and are designed to cover the entire cornea, plus a portion of the sclera, the white of the eye.
Hybrid Contact Lenses: Hybrid contacts are RGP lenses that are surrounded by a soft lens lining or skirt.
Intacs® Corneal Implants: Intacs consist of micro-thin corneal implants designed for the reduction or elimination of myopia and astigmatism in patients with keratoconus. Intacs are thin plastic, semi-circular rings, which are surgically inserted under the surface of the cornea. When inserted into the keratoconic cornea, they flatten the cornea, changing its shape. The placement of Intacs may reduce corneal irregularities caused by keratoconus.
Corneal Transplant Surgery: In keratoconus, when sufficient vision can no longer be achieved by contact lenses due to steepening of the cornea, scarring, or lens intolerance, a corneal transplant may be the only option. The surgery is generally performed as an outpatient procedure with either general or local anesthesia. During the surgery, the part of the cornea affected by keratoconus is removed and replaced with a donor cornea. While the surgical transplantation of a new cornea will resolve the basic problem of corneal surface irregularity, eyeglasses or contact lenses are usually needed after the surgery for vision correction. It’s possible that over time multiple transplants may be required.
Diagnostic Tools
Corneal Topography: Corneal topography is an imaging technique that is used to create a color-coded map of the curvature of the cornea using a specialized camera and computerized analysis. This information allows your doctor to assess whether there are any abnormalities in corneal shape that may indicate keratoconus or other disorders. Additionally, corneal topography can provide information that is useful in fitting a contact lens to the unique shape of the cornea.
Corneal Tomography: Corneal tomography also provides a map of the front surface, as well as additional information about the curvature of the back surface of the cornea (inside of the eye). Corneal tomography may also be used to create a map showing the thickness of different areas of the cornea.
Kmax (maximum keratometry): This parameter indicates the highest degree of steepening within the imaged corneal surface
Keratometry: The curvature measurement of the front surface of the cornea
Pachymetry: The process of measuring the thickness of the cornea
Eye Care Professionals

Optometrist: Optometrists are eyecare professionals who provide primary vision care, which can range from vision testing and optical correction to disease diagnosis, treatment, and management. Optometrists may diagnose keratoconus in their own office or refer to ophthalmologists for additional diagnostic testing. Optometrists provide fittings for contact lenses and glasses, both before and after treatments, such as corneal cross-linking. While all optometrists receive training in contact lens fitting, some undergo additional training to become contact lens specialists, meaning that they can fit their patients with more customized or complex specialty lens designs, such as scleral lenses and RGP lenses.
Optician: Opticians are technicians who are trained to design, verify and fit glasses, contact lenses, and other corrective devices. Opticians do not diagnose and treat eye diseases or write prescriptions. They use prescriptions supplied by optometrists or ophthalmologists to create appropriate corrective lenses for patients.
Ophthalmologist: An ophthalmologist is a medical or osteopathic doctor who specializes in eye care. An ophthalmologist can diagnose and treat eye diseases and perform surgery, like corneal transplants or LASIK. They can also perform less-invasive treatments, such as corneal cross-linking. Both optometrists and ophthalmologists can also be involved in scientific research on causes and cures for eye diseases and vision disorders.
